Spinal cord: Cross section and tracts
The spinal cord is 45 cm long in the adult, a measurement it shares with the lengths of the femur and the vas deferens and with the distance from the lips to the oesophagogastric junction.
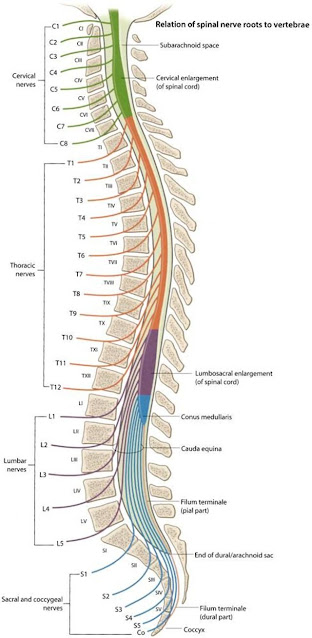
It has an elongated cylindrical shape but is somewhat flattened antero - posteriorly, especially in the lumbar region. The cylinder is not uniform in diameter, but bears cervical and lumbar enlargements that correspond to the origins of the brachial and lumbosacral plexuses.
The spinal cord is divided into 31 segments, each emitting a pair of spinal nerves. There are:
Eight cervical segments.
Twelve thoracic segments.
Five lumbar segments.
Five sacral segments.
One coccygeal segment.
With the exception of C1 and C2, the spinal nerves exit the spinal canal through the intervertebral foramina.
At the terminal end of the spinal cord:
The conus medullaris is the tapered terminal portion of the cord.
The cauda equina is the collection of spinal nerves that continue inferiorly in the spinal canal after the cord has ended, until they reach their respective intervertebral foramina.
The filum terminale, continues down to become attached to the coccyx. The filum terminale is mainly pia mater invested in a sheath of dura, but it does contain a prolongation of the central canal of the cord in its upper part.
Table gives the approximate levels of the cord segments. As a rough guide, allow one segment difference in the cervical cord, two in the upper thoracic, three in the lower thoracic and four or five in the lumbar and sacral cord.
Following the injection of local anaesthetics or other fluids intrathecally, the spread will be influenced in part by the curvature of the spinal canal. When hyperbaric solutions are used, the local anaesthetic will tend to gravitate towards the lowest part of spine, i.e. to the bottom of the kyphosis.
In the supine non-pregnant adult, these levels are L4 in the lumbar region and T8 in the thoracic region.
In the pregnant patient, these levels are L4–5 and T6, the latter being, incidentally, an ideal dermatomal height for regional anaesthesia for caesarean section.
As the afferent nerve fibres are progressively added to the cord from below upwards and the efferent fibres are progressively given off from above downwards, the amount of white matter declines progressively from the cervical down to the lumbar region. The grey matter is greatly increased in both the cervical and lumbar enlargements, which correspond to the zones of origin of the motor nerves to the upper and lower limbs.
The central canal continues downwards from the 4th ventricle as a narrow tube, lined with ciliated ependymal cells and containing CSF. It traverses the whole length of the cord, dilates somewhat within the conus medullaris, and continues for a short distance within the filum terminale.
Cross-sectional anatomy of the spinal cord
In cross-section, the spinal cord is approximately oval, with a deep anterior median fissure and a shallow posterior median sulcus, from which a glial posterior median septum extends about halfway into the substance of the cord.
The anterior nerve roots, in contrast, emerge by a number of nerve tufts and their line of origin is not marked by a groove along the cord.
The centre of the cord contains an approximately ‘H’-shaped area of grey matter, surrounded by white matter:
The grey matter contains unmyelinated axons and the cell bodies of interneurons and motor neurons. Located in the centre of the grey matter is the CSF-containing central canal. The points of the ‘H’ correspond to the dorsal and ventral (posterior and anterior) horns. There are also lateral horns in the thoracic region of the cord, which correspond to pre-ganglionic sympathetic neurons.
The white matter contains columns of myelinated axons, called tracts. These tracts are organised into:
- Ascending tracts, containing sensory axons;
- Descending tracts, containing motor axons.
The spinal cord enlarges in two regions:
- The cervical enlargement at C4–T1, corresponding to the brachial plexus, which innervates the upper limbs
- The lumbar enlargement at L2–S3, corresponding to the lumbar plexus, which innervates the lower limbs.
The most important ascending tracts:
The dorsal (posterior) columns contain axons of nerves concerned with proprioception (position sense), vibration and two-point discrimination (fine touch), which is capped by the substantia gelatinosa.
The anterior and lateral spinothalamic tracts carry sensory information about pain, temperature, crude touch and pressure.
The anterior and posterior spinocerebellar tracts carry proprioceptive information from the muscles and joints to the cerebellum.
The most important descending tracts:
The anterior and lateral corticospinal tracts, also known as the pyramidal tracts, carry the axons of upper motor neurons. In the ventral horn of the spinal cord, these axons relay to α-motor neurons (or lower motor neurons) that innervate muscle.
The extrapyramidal tracts: rubrospinal, tectospinal, vestibulospinal, olivospinal and reticulospinal tracts. The extrapyramidal neurons originate at brainstem nuclei and do not pass through the medullary pyramids. Their primary role is in the control of posture and muscle tone.

Sensory afferent pathways
- Sensory receptors, which encode stimuli by repetitive firing of action potentials. The different sensory receptor types are specific to their sensory modalities: proprioceptors, nociceptors, thermoreceptors and mechanoreceptors relay sensory information concerning limb position, tissue damage (potentially causing pain), temperature and touch, respectively. The perception of the stimulus is dependent upon the neuronal pathway rather than the sensory receptor itself. For example, pressing on the eye activates the optic nerve and gives the impression of light, despite the stimulus being pressure rather than photons.
- First-order neurons transmit action potentials from sensory receptors to the spinal cord, where they synapse with second-order neurons. These neurons are pseudounipolar, with their cell bodies located in the dorsal root ganglion, a swelling of the dorsal root just outside the spinal cord.
- Second-order neurons conduct action potentials to the thalamus, where they synapse with third-order neurons.
- Third-order neurons relay action potentials to the cerebral cortex via the internal capsule.
- The primary somatosensory cortex is the area of the cerebral cortex that receives and performs an initial processing of the sensory information. It is organised in a somatotropic way with specific areas of cortex dedicated to specific areas of the body, known as the sensory homunculus. Of note: the hands and lips make up a major component, reflecting their tactile importance.
There are two major pathways by which sensory information ascends in the spinal cord:
The dorsal column–medial lemniscal (DCML) pathway
carries sensory information about two point discrimination, vibration and proprioception. The name of the pathway comes from the two structures through which the sensory signals pass: the dorsal columns of the spinal cord and the medial lemniscus in the brainstem.
– The first-order neuron is extremely long. It enters the dorsal root of the spinal cord and ascends in the dorsal columns on the same side (ipsilateral). Sensory neurons from the lower body travel in the medial fasciculus gracilis of Goll and synapse in the gracile nucleus in the medulla oblongata, whilst sensory neurons from the upper body travel in the lateral fasciculus cuneatus of Burdach and synapse in the cuneate nucleus.
– In the medulla, first-order neurons synapse with second-order neurons, which then cross over to the contralateral side and ascend to the thalamus. After this sensory decussation, the fibres ascend through the brainstem in a tract called the medial lemniscus.
The spinothalamic tract
carries sensory information about crude touch, pressure, temperature and pain. In contrast to the DCML pathway, the spinothalamic tract crosses the midline at the level of the spinal cord rather than the medulla:
– The first-order neurons enter the dorsal root of the spinal cord and may ascend or descend one or two vertebral levels (along Lissauer’s tract) before synapsing with second-order neurons in the dorsal horn at substantia gelatinosa.
– The axons of the second-order neurons decussate anterior to the central canal of the spinal cord, in an area called the anterior commissure, before ascending to the thalamus in the contralateral spinothalamic tract.

The pain and temperature fibres are contained in the lateral spinothalamic tract, within the lateral white substance anterior to the pyramidal tract.
The tactile fibres lie within the anterior spinothalamic tract, immediately anterior to the tip of the anterior horn of the grey matter.
The corticospinal tract
• The motor cortex, located in the pre-central gyrus. This area is the brain’s final common output, resulting in the initiation of movement.
• An upper motor neuron, which originates in the motor cortex and descends through the spinal cord within the corticospinal tract:
– Upper motor neurons travel through the posterior limb of the internal capsule.
– At the level of the pons, a significant proportion of upper motor neurons synapse in the pontine nuclei, forming the ventral part of the pons. These postsynaptic fibres then travel posteriorly to reach the cerebellum through the middle cerebral peduncle.
– At the medullary pyramids, 90% of the remaining nerve fibres decussate and descend in the lateral corticospinal tract of the spinal cord.
– The 10% of nerve fibres that do not decussate descend in a separate ipsilateral tract: the anterior corticospinal tract.
– When they have reached their intended vertebral level in the spinal cord, the upper motor neurons synapse with lower motor neurons in the ventral horn of the spinal cord.
• A lower motor neuron, which leaves the CNS to innervate skeletal muscle. There are two types of lower motor neuron:
– α-motor neurons leave the anterior horn, forming the spinal nerve. The spinal nerve exits the spinal canal via the intervertebral foramen, becoming a peripheral nerve. Ultimately, the α-motor neuron innervates extrafusal fibres of skeletal muscle, causing muscle contraction.
– γ-motor neurons innervate the intrafusal fibres of skeletal muscle (the ‘muscle spindles’), which are involved in proprioception.





Comments
Post a Comment
Please share your views and comments in the comment section. Give your opinion if there is anything to update.
Subscribe the channel to get updates regarding regular blog post.
Share the content if you think its appropriate.
Thank you.