EPIDURAL TEST DOSE: WHAT and WHY
INTRODUCTION
Central Neuraxial block (CNB) is the most popular and most widely practiced technique amongst all anaesthetic techniques. Report and findings of the 3rd National Audit Project of the Royal College of Anaesthetists showed in a conservative estimate, that CNB is used for at least 8–10% of all operations in the UK.
Central Neuraxial block (CNB) techniques can produce highly effective pain relief for a wide variety of indications and may decrease patient morbidity after major surgery. Individual studies and meta-analyses have examined this effect and suggested benefit, [1–2] with even cautious commentators accepting that there is merit in the suggestion.[3] Yeager’s very small study reporting that epidural analgesia markedly reduced complication rates (overall complications, cardiovascular failure, major infections, cortisol rise) in high-risk patients was one of the earlier studies to suggest benefits out with improved analgesia. [4] Rodgers metanalysis [5] reported a reduction in deep vein thrombosis (DVT) by 44%, pulmonary embolism (PE) by 55%, transfusion requirements by 50%, pneumonia by 39%, and respiratory depression by 59%, all statistically significant effects. There were also non-significant reductions in myocardial infarction and renal failure.
Serious and permanent complications of neuraxial anesthesia are very rare. In a prospective audit report from the UK, the incidence of permanent injury from neuraxial anesthesia was 4.2 per 100,000 [7]. This report also highlighted that most injuries resolved within six months.
Among all the complications and adverse effects
of regional anaesthesia, the reported incidence of major LAST events (i.e.,
seizures or cardiac arrest) is very low. Major LAST events have decreased
markedly since the early 1980s, likely related to increased awareness and
routine incorporation of preventive measures into clinical practice. [8,9]
Local anesthetic systemic toxicity (LAST) is a potentially devastating but rare complication of regional anesthesia. Estimating the frequency of LAST events in the context of peripheral nerve blocks (PNBs) is challenging due to their infrequent occurrence as well as the range of their attendant clinical signs and symptoms of LAST. Local anesthetic systemic toxicity (LAST) can occur with any route of administration of local anesthetics but is much less likely with spinal than with epidural anesthesia, because such a small dose of local anesthetic (LA) is injected for spinal anesthesia. LAST is a rare but potentially lethal event, that may consist of central nervous system and/or cardiovascular effects ranging from minor manifestations (eg, perioral numbness, tinnitus, twitching), to major events, including seizures, coma, severe hypotension, arrhythmias, and asystole. LAST occurs most commonly with inadvertent intravascular injection of LA with almost immediate onset of signs and symptoms, but delayed onset may also occur with epidural infusion after systemic absorption of LA or migration of the catheter into a blood vessel.
Association between Plasma concentration of Lidocaine and Side effects:
|
Plasma Concentration |
Possible side effects |
|
4-6 µg/mL |
Lightheadedness, numb tongue, metallic taste,
increased blood pressure, dizziness. |
|
8 µg/mL |
Visual and auditory disturbances,
dissociation, muscle twitching, decreased blood pressure. |
|
12 µg/mL |
Convulsions (Benzodiazepines sensitive) |
|
16 µg/mL |
Come |
|
20 µg/mL |
Respiratory arrest |
|
24 µg/mL |
Cardiovascular system depression/Collapse |
Recent estimates demonstrate a low incidence and suggest a decreasing rate trend; however, most of these studies have been determined from regional anesthesia registries and single institution quality improvement or billing queries, thus lacking generalizability to national practice. [10-13] A recent study using a United States database found the incidence of LAST was 1.8/1,000 PNBs, noticeably higher than previous estimates.[14] However, this study did not directly identify a diagnosis of LAST but used the presence of surrogate outcomes, such as a diagnosis of seizure, or cardiac arrest and administration of Intralipid, to identify the incidence of LAST.[14] The results lead to a question of whether improvements in technique, utilization of ultrasound guidance and awareness of LAST have led to decreases in the rate of LAST in the United States.
Smaller quantities of local anaesthesia can produce blood levels above the seizure threshold if injected intravenously or intra arterially in the cerebral circulation (A seizure threshold is a person's likelihood to have a seizure. The higher the threshold the less likely it is that a seizure will happen).
Frequent aspiration, careful fixation of the needle, careful test doses and incremental injections are clearly indicated whenever injections are made near blood vessels, thereby early detection and prompt action is the key to prevent perioperative mortality associated with LAST.
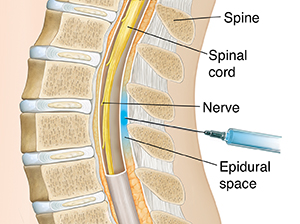
Before initiating an epidural local anaesthetic infusion, a test dose may be administered. A test dose [15] is the injection of a quantity of drug sufficient to produce some reliable subtoxic clinical sign if injected intrathecally or intravascularly. The purpose of this test is to exclude the misplacement of the epidural catheter.
A small volume of lidocaine 1.5% with epinephrine is traditionally used for this purpose. If the catheter is in a blood vessel, the injection of a small volume of an epinephrine solution will result in a tachycardia. This is not without a risk in the patient with severe heart disease. If the catheter lies in the subarachnoid space, then the injection of a dose of local anaesthetic similar to that used in intrathecal anaesthesia should result in a sudden onset of loss of sensation and weakness in the legs in the awake patient. Hypotension may also develop swiftly. [15]
Till now it is the most reliable and practical test for early recognition of LAST.
The reliable indicators of intravascular injection are- [16]
- The tachycardia produced by 15 µgm epinephrine injected intravenously.
- Increase in Heart rate by 30% (from 80-110 beats per minute) and Increase in systolic blood pressure (SBP) by 15 mmHg.

- Within
20 seconds following
injection.
- The
increase is transient.
- Changes return towards normal within
60 seconds.
A mechanical beat to beat pulse counting device is essential rather than a manual count.
Criteria for Epinephrine Test Doses:
|
Situation |
Hemodynamic criteria |
||
|
Normal patient |
HR increase >20 bpm |
||
|
SBP increase >15 mmHg |
|||
|
Beta blockade |
HR- no change |
||
|
SBP increase >15 mmHg |
|||
|
Advanced age |
HR increase >9 bpm |
||
|
SBP increase >15 mmHg |
|||
|
General anaesthesia |
HR increase >8 bpm |
||
|
SBP increase >13 mmHg |
HR- Heart rate, SBP- Systolic blood pressure,
BPM- Beats per minute
There are several limitations, thus multiple safety steps are always important to the test-
- Patients receiving beta blocking drugs will not respond
with a tachycardia and changes in systolic blood pressure, so will need to
be monitored or an alternative test used.
- Elderly patients may also have a reduced response to
epinephrine.
- Pre medicated patients cannot be relied on to report
subjective clinical signs.
- General anaesthesia will also reduce the response to
epinephrine by 50%.
Alternative tests:[16]
- Doses of 100mg chloroprocaine, 100mg lidocaine or 25mg
bupivacaine injected intravenously will produce subjective signs and may
be a reliable substitute in this situation.
- Another alternative is the injection of 1 ml of air
while monitoring the heart sounds with a precordial doppler stethoscope.
This has been used in obstetric anaesthesia, but it may not be practical
in the operating room.
References:
1. Ballantyne JC, Carr DB, deFerranti S, et al. The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analysis of randomized controlled trials. Anesth Analg 1998;86:598–612.
2 Rodgers A et al. Reduction of postoperative mortality and
morbidity with epidural or spinal anaesthesia: Results of overview of
randomized trials. Br Med J 2000;321:1493–1497.
3 Buggy DJ, Smith G. Epidural anaesthesia and analgesia:
better outcome after major surgery? Growing evidence suggests so. Br Med J
1999;319:530–531.
4.Yeager MP et al. Epidural anesthesia and analgesia in
high-risk surgical patients. Anesthesiology 1987;66:729–736.
5. Rodgers A et al. Reduction of postoperative mortality and
morbidity with epidural or spinal anaesthesia: results from overview of
randomized trials. Br Med J 2000;321:1493.
6. Cooper GM, McClure JH. Anaesthesia. Chapter 9 in: Why
Mothers Die: Sixth Report of the Confidential Enquiries into Maternal Deaths in
the United Kingdom. RCOG Press, London 2004
10. Sites BD, Taenzer AH, Herrick MD, et al. Incidence of
local anesthetic systemic toxicity and postoperative neurologic symptoms
associated with 12,668 ultrasound-guided nerve blocks: an analysis from a
prospective clinical registry. Reg Anesth Pain Med. 2012;37:478–482. [PubMed]
[Google Scholar]
11. Orebaugh SL, Kentor ML, Williams BA. Adverse outcomes
associated with nerve stimulator-guided and ultrasound-guided peripheral nerve
blocks by supervised trainees: update of a single-site database. Reg Anesth
Pain Med. 2012;37:577–582. [PMC free article]
[PubMed]
[Google Scholar]
12. Barrington MJ, Kluger R. Ultrasound guidance reduces the
risk of local anesthetic systemic toxicity following peripheral nerve blockade.
Reg Anesth Pain Med. 2013;38:289–299. [PubMed]
[Google Scholar]
13. Liu SS, Ortolan S, Sandoval MV, Curren J, Fields KG,
Memtsoudis SG, YaDeau JT. Cardiac arrest and seizures caused by local
anesthetic systemic toxicity after peripheral nerve blocks: should we still
fear the reaper? Reg Anesth Pain Med. 2016;41:5–21. [PubMed]
[Google Scholar]
14. Mörwald EE, Zubizarreta N, Cozowicz C, Poeran J, Memtsoudis
SG. Incidence of local anesthetic systemic toxicity in orthopedic patients
receiving peripheral nerve blocks. Reg Anesth Pain Med. 2017;42:442–445. [PubMed]
[Google Scholar]
15. Wylie and Churchill- Davidson's A Practice of
Anaesthesia. Regional anaesthetic techniques, 2003;37: 614.


Extremely useful information which you have shared here. This is a great way to enhance knowledge for us, and also helpful for us. Thankful to you for sharing an article like this. physio for plantar fasciitis.
ReplyDelete